Establishing a diagnosis of migraine
The criteria for diagnosing migraine are outlined in the International Classification of Headache Disorders (ICHD) IIIβ. Migraine diagnosis is based on clinical history and examination rather than through laboratory and/or radiological investigation.1 There are three common primary headache disorders—migraine, episodic tension-type headache (ETTH), and cluster headache—that are often characterized by recurrent headache.2 Migraine and ETTH can also be chronic, occurring more than 15 days per month, and may have no pain-free periods. Migraine can begin at puberty, and commonly occurs between the ages of 35 and 45 years.2
Primary care providers (PCPs) have historically been provided with limited education on the diagnosis and management of headache.3 Once a diagnosis of migraine has been made, it is accurate 98% of the time. However, migraine is often not diagnosed (up to a quarter of the time), resulting in inappropriate management. Worldwide, only 40% of migraine sufferers have been given a professional diagnosis.2,4 On average, there is more than a four-year delay between diagnosing migraine and beginning prophylaxis.3
Migraine Without Aura
Table 1: International Classification of Headache Disorders (ICHD) diagnostic criteria for migraine.5
| A: At least five attacks1 fulfilling criteria B-D |
| B: Headache attacks lasting 4-72 hr (untreated or unsuccessfully treated)2,3 |
| C: Headache has at least two of the following four characteristics:
1. Unilateral location 2. Pulsating quality 3. Moderate or severe pain intensity 4. Aggravation by or causing avoidance of routine physical activity (eg, walking, climbing stairs) |
| D: During headache at least one of the following:
1. Nausea and/or vomiting 2. Photophobia and phonophobia |
| E: Not better accounted for by another ICHD-3 diagnosis. |
Footnotes
- One or a few migraine attacks may be difficult to distinguish from symptomatic migraine-like attacks and the nature of a single or a few attacks may be difficult to understand. Therefore, at least five attacks are required. Individuals who otherwise meet criteria for 1.1 Migraine without aura but have had fewer than five attacks should be coded 1.5.1 Probable migraine without aura.
- When the patient falls asleep during migraine and wakes up without it, duration of the attack is reckoned until the time of awakening.
- In children and adolescents (<18 years), attacks may last 2-72 hours (the evidence for untreated durations of less than two hours in children has not been substantiated).
Migraine With Aura
These are recurrent attacks, lasting minutes, of unilateral fully-reversible visual, sensory or other CNS symptoms. They usually develop gradually and are typically followed by headache and associated migraine symptoms.
Table 2: International Classification of Headache Disorders (ICHD) diagnostic criteria for migraine with aura.6
| A: At least two attacks fulfilling criteria B and C |
| B: One or more of the following fully reversible aura symptoms:
1. Visual 2. Sensory 3. Speech and/or language 4. Motor 5. Brainstem 6. Retinal |
| C. At least three of the following six characteristics:
1. At least one aura symptom spreads gradually over ≥5 minutes 2. Two or more aura symptoms occur in succession 3. Each individual aura symptom lasts 5-60 minutes1 4. At least one aura symptom is unilateral2 5. At least one aura symptom is positive3 6. The aura is accompanied, or followed within 60 minutes, by headache |
| E: Not better accounted for by another ICHD-3 diagnosis. |
Footnotes:
- When, for example, three symptoms occur during an aura, the acceptable maximal duration is 3×60 minutes. Motor symptoms may last up to 72 hours.
- Aphasia is always regarded as a unilateral symptom; dysarthria may or may not be.
- Scintillations and pins and needles are positive symptoms of aura.
Chronic Migraine
Chronic migraine occurs on 15 or more days/month for more than 3 months, which, on at least 8 days/month, has the features of migraine headache.
Table 3: International Classification of Headache Disorders (ICHD) diagnostic criteria for chronic migraine.7
| A: Headache (migraine-like or tension-type-like1) on ≥15 days/month for >3 months, and fulfilling criteria B and C |
| B: Occurring in a patient who has had at least five attacks fulfilling criteria B-D for Migraine without aura and/or criteria B and C for Migraine with aura |
| C: On ≥8 days/month for >3 months, fulfilling any of the following2:
1. Criteria C and D for Migraine without aura 2. Criteria B and C for Migraine with aura 3. Believed by the patient to be migraine at onset and relieved by a triptan or ergot derivative |
| D: Not better accounted for by another ICHD-3 diagnosis3;4;5 |
Footnotes:
- The reason for singling out Chronic migraine from types of episodic migraine is that it is impossible to distinguish the individual episodes of headache in patients with such frequent or continuous headaches.
- Characterization of frequently recurring headache generally requires a headache diary to record information on pain and associated symptoms day-by-day for at least one month.
- Because tension-type-like headache is within the diagnostic criteria for Chronic migraine, this diagnosis excludes the diagnosis of Tension-type headache or its types.
- New daily persistent headache may have features suggestive of Chronic migraine. The latter disorder evolves over time from Migraine without aura and/or Migraine with aura.
- The most common cause of symptoms suggestive of chronic migraine is medication overuse, as defined under Medication-overuse headache. Around 50% of patients apparently with Chronic migraine revert to an episodic migraine type after drug withdrawal; such patients are in a sense wrongly diagnosed as Chronic migraine. Equally, many patients apparently overusing medication do not improve after drug withdrawal; the diagnosis of 8.2 Medication-overuse headache may be inappropriate for these.
For additional information on migraine diagnosis, including specific ICHD-3 coding, please visit references 5-7 below.
Headache history: useful questions
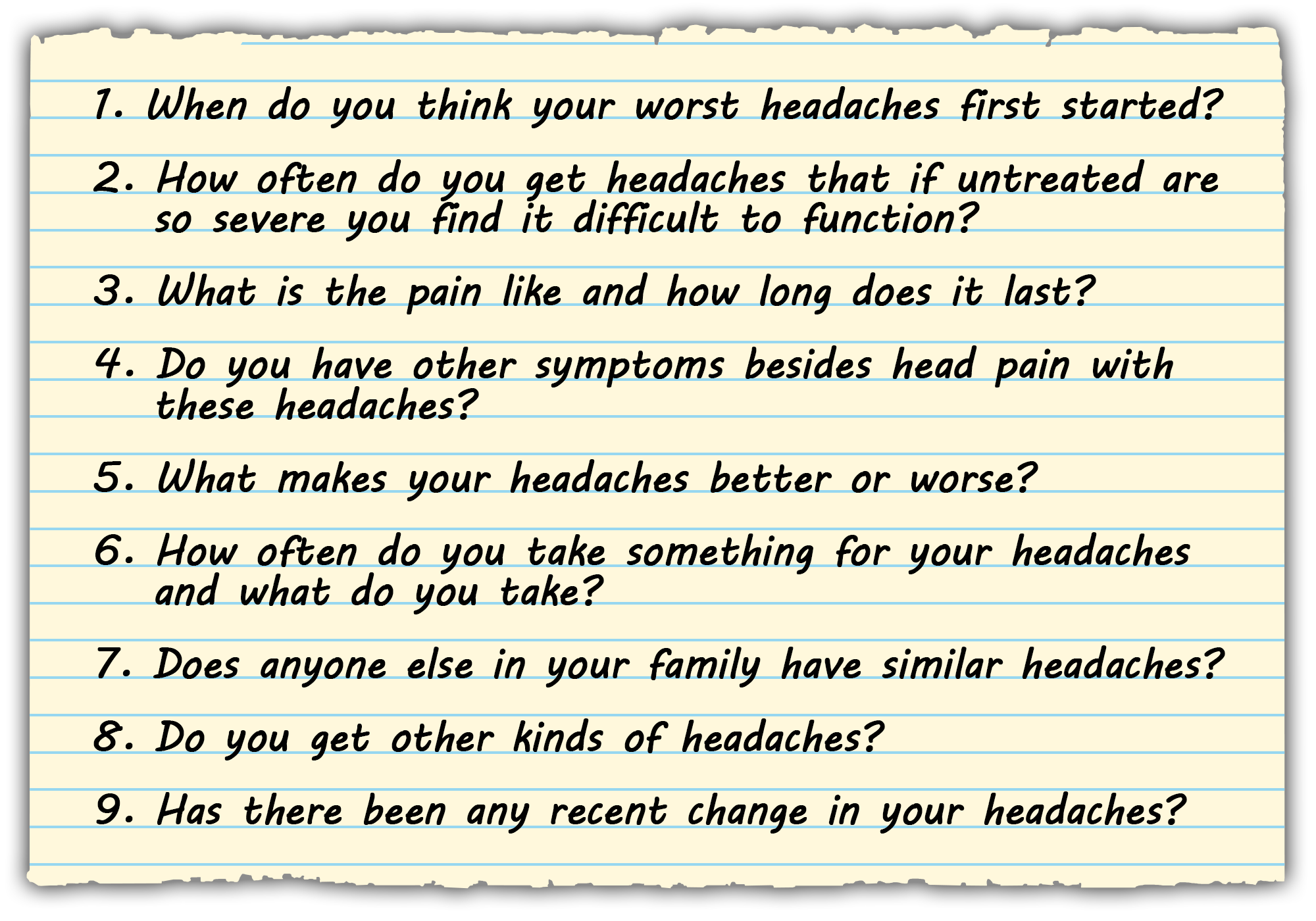
A headache diary can be helpful in detecting medication overuse, documenting the frequency and severity of headaches, establishing triggers (eg, dietary triggers, missed meals, emotional stress, and smells), monitoring medication use and the response to therapy, and identifying any association between headaches and stage of the menstrual cycle.4,8
Is it migraine or an ETTH?
ETTH is the most common headache type and can occur at any age. Most people with this condition self-medicate with over-the-counter analgesics. Differentiating between migraine and ETTH is a common diagnostic challenge for PCPs. In ETTH, the pain is bilateral, of mild-to-moderate severity, tight, pressing, and band-like; there can be associated neck or jaw discomfort. ETTH pain is rarely throbbing or unilateral and is not aggravated by exertion. With ETTH, there are no associated symptoms of prodrome or aura; however, there can be anorexia without nausea or vomiting.4 Table 4 summarizes differences between the clinical presentation of migraine and ETTH.
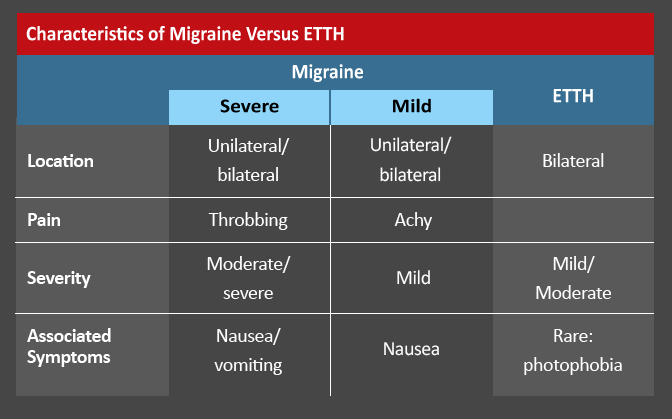
Table 4: Characteristics of Migraine vs ETTH
Cluster headache
Cluster headache is characterized by unilateral severe headache attacks. The pain is orbital, supraorbital or temporal and lasts for 15–180 minutes. Accompanying and on the same side as the pain there is at least one of lacrimation, eyelid edema, ptosis, miosis, rhinorrhea, nasal congestion, forehead and/or facial sweating.9 Cluster headache occurs seasonally for 80% of sufferers, and it is 5-6 times more common in men. Attacks typically begin between 20 and 50 years of age. In episodic cluster headache, attacks occur in “cluster” periods that last between 6 and 12 weeks followed by periods of remission. In chronic cluster headache attacks occur without remission. Cluster headache can be triggered by alcohol, exercise, histamine, and nitroglycerine.9
Excluding secondary causes of headache and the role of head imaging
Best practice is a clinical evaluation to exclude secondary causes of headache, such as head injury, subarachnoid hemorrhage, and brain tumor through a thorough history and neurological examination.10 Neuroimaging is indicated where there are ominous clinical features and a secondary cause of headache is suspected.
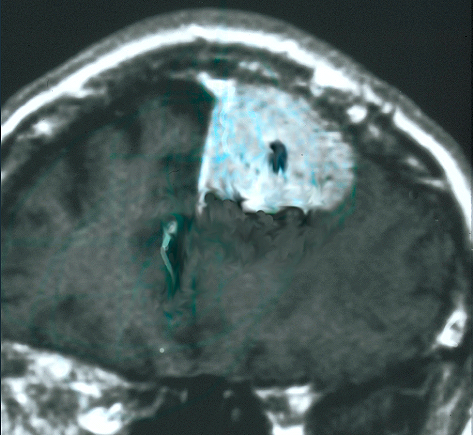
Recent evidence suggests that computed tomography (CT) and magnetic resonance imaging (MRI) are overused in the assessment of migraine sufferers.11 The American Headache Society recommends that neuroimaging studies not be performed in migraine sufferers who have a stable headache that meets the criteria for migraine,12 and the American College of Radiology recommends that imaging should not be performed for an uncomplicated headache.
There is insufficient evidence regarding the role of diagnostic imaging in patients presenting with atypical headaches; further research is required in order to provide clinicians with appropriate evidence-based guidance.11 Other diagnostic tests, including blood work or a lumbar puncture, are occasionally performed to exclude secondary sources of headache.
References
- International Classification of Headache Disorders (ICHD) III criteria. (ichd-3.org/) Accessed 9/25/18.
- World Health Organization. Headache. WHO fact sheets. (int/mediacentre/factsheets/fs277/en) Accessed 9/25/18.
- Minen MT, Loder E, Tishler L, Silbersweig D. Migraine diagnosis and treatment: a knowledge and needs assessment among primary care providers. 2016;36:358-370.
- Sinclair AJ, Sturrock A, Davies B, Matharu M. Headache management: pharmacological approaches. Pract Neurol. 2015;15:411-423.
- IHS Classification ICHD-3. Migraine Without Aura. Available at: https://www.ichd-3.org/1-migraine/1-1-migraine-without-aura/. Accessed 9/25/18.
- IHS Classification ICHD-3. Migraine With Aura. Available at: https://www.ichd-3.org/1-migraine/1-2-migraine-with-aura/. Accessed 9/25/18.
- IHS Classification ICHD-3. Chronic Migraine. Available at: https://www.ichd-3.org/1-migraine/1-3-chronic-migraine/. Accessed 9/25/18.
- Dougherty C, Silberstein SD. Providing care for patients with chronic migraine: diagnosis, treatment, and management. Pain Pract. 2015;15:688-692.
- Leone M, Giustiniani A, Cecchini AP. Cluster headache: present and future therapy. Neurol Sci. 2017; 38(S1):45–50.
- Starling AJ, Dodick DW. Best practices for patients with chronic migraine: burden, diagnosis, and management in primary care. Mayo Clin Proc. 2015;90:408-414.
- Minen MT, Tanev K, Friedman BW. Evaluation and treatment of migraine in the emergency department: a review. . 2014;54:1131-1145.
- ABIM Foundation Choosing Wisely Campaign (www.choosingwisely.org/doctor-patient-lists/) Accessed on 9,25,18.
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
 Copyright © 2024 Med Learning Group. Built by
Copyright © 2024 Med Learning Group. Built by